Coronary artery disease
Coronary artery disease, often commonly referred to as coronary artery disease, is one of the greatest challenges of modern medicine and public health. In order to fully understand its essence, it is necessary to precisely define the key concepts. Ischaemic heart disease (IHD) is a broad term that encompasses all conditions in which there is an insufficient supply of oxygen and nutrients to the heart muscle. Coronary artery disease (CVD), on the other hand, is the most common cause of IHD, accounting for more than 98% of cases, and refers specifically to ischemic conditions resulting from changes in the coronary arteries – vessels that wrap around the heart like a wreath and supply it with blood.
Table of contents
What is and causes of coronary artery disease
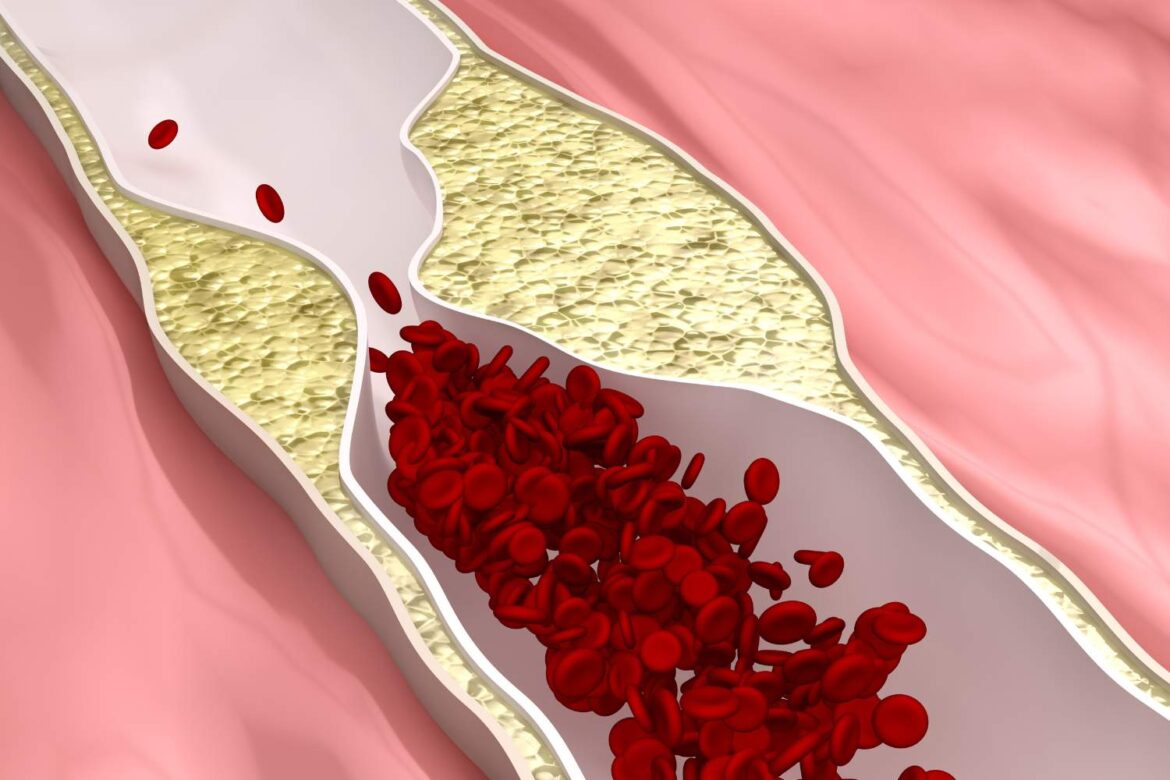
The foundation of coronary artery disease is atherosclerosis, an insidious and long-term disease process during which the so-called atherosclerotic plaques form on the inner walls of the arteries. These are complex structures consisting mainly of cholesterol, inflammatory cells, fibrin and calcifications, which gradually narrow the lumen of the vessel, hindering blood flow.
The scale of the problem in Poland is alarming. According to current data from the National Health Fund (NFZ), about 2 million Poles suffer from ischemic heart disease, which is 5.5% of the country’s population. Although mortality rates from IHD have fallen by more than 50% in the last two decades, thanks to advances in medicine, the condition still remains one of the leading causes of death in Europe, accounting for around 20% of all deaths. The huge burden on the healthcare system is illustrated by the costs – in 2023, the National Health Fund allocated nearly PLN 3.8 billion for the reimbursement of CVD-related services.
However, the analysis of epidemiological data reveals a certain paradox of progress in cardiology. On the one hand, we are observing a decrease in mortality due to acute incidents, such as myocardial infarction, which is an undoubted success of interventional cardiology and quick access to treatment. On the other hand, the number of patients with chronic diseases, especially heart failure, is increasing. This is not a contradiction. Modern treatments, such as immediate coronary angioplasty, save the lives of patients who in the past would not have had a chance of surviving a heart attack. However, these patients are often left with permanently damaged heart muscle, with post-infarction scarring, which impairs its function. Over time, this leads to the development of chronic heart failure. Data from the National Health Fund indicate that the probability of heart failure within 7 years of a heart attack is as high as 50%. In this way, by saving lives in the acute phase, medicine faces the challenge of caring for an increasing population of patients requiring long-term, expensive treatment due to complications. This phenomenon highlights the fundamental importance of comprehensive secondary prevention, rehabilitation and coordinated care programmes such as KOS-Infarction in the diagnosis of ischaemic heart disease.
Causes and Risk Factors – Who Is at Risk for Coronary Artery Disease?
The development of coronary artery disease is a complex process that is influenced by many factors. They can be divided into those that we can influence (modifiable) and those that we cannot change (non-modifiable). It is crucial to understand that these factors do not operate in isolation, but create a network of interconnections, intensifying their negative impact.
Modifiable risk factors: What can you change to protect your heart?
The foundation on which most cardiac problems develop is an unhealthy lifestyle. It leads to the development of clinical risk factors that directly accelerate the atherosclerotic process.
- Smoking: Both active and passive smoking is one of the most dangerous enemies of the circulatory system. The substances contained in tobacco smoke directly damage the endothelium (the inner lining of vessels), promote thrombotic processes and rapidly accelerate the development of atherosclerosis.
- Hypertension: Persistent high blood pressure causes constant, mechanical “wear” of the arteries, making them more susceptible to damage and rupture of atherosclerotic plaques.
- Lipid disorders: Elevated LDL (low-density lipoprotein) cholesterol, commonly known as “bad cholesterol”, is a key building block of atherosclerotic plaque. LDL particles penetrate the artery wall, where they oxidize and initiate the inflammatory process.
- Diabetes and insulin resistance: High blood glucose levels (hyperglycemia) and elevated insulin levels have a toxic effect on the walls of blood vessels, intensifying inflammation and accelerating atherosclerosis. Coronary artery disease is the most common complication of diabetes.
- Overweight and obesity: They are the “mother” of many other risk factors. Excessive body weight, especially abdominal obesity, often leads to the development of hypertension, insulin resistance, type 2 diabetes and lipid disorders.
- Lack of physical activity and an unhealthy diet can lead to elevated cholesterol levels, which increases the risk of myocardial infarction. A sedentary lifestyle and a diet rich in saturated fats, trans fats and simple sugars, and low in vegetables, fruits and fiber, are the basis for the development of all of the above factors.
- Chronic stress and psychosocial factors: Type A personality, characterized by constant competition and pressure, as well as chronic stress, lead to overactivation of the sympathetic nervous system and increased levels of stress hormones (e.g., cortisol), which negatively affects the heart and vessels.
Nonmodifiable risk factors: Effects of age, sex, and genetics
- Age: The risk of developing coronary artery disease increases with age, becoming significant after the age of 40.
- Sex: Statistically, men get sick earlier. However, in women, the risk increases rapidly after menopause, which is associated with the loss of the protective effect of estrogen on the cardiovascular system.
- Genetic factors: The presence of coronary artery disease or myocardial infarction at a young age (55 years in men <, 65 years in women <) in first-degree relatives (parents, siblings) is a strong, independent risk factor.
Lesser-known but significant risk factors and rare causes of CVD
Modern medicine perceives atherosclerosis not only as a cholesterol-related disease, but above all as a chronic inflammatory process influenced by many systemic factors.
- Chronic inflammation: Elevated levels of C-reactive protein (CRP) in the blood, which is a marker of inflammation, are considered an independent risk factor for cardiovascular events. Autoimmune diseases such as rheumatoid arthritis (RA) significantly accelerate the development of atherosclerosisand increase the risk of heart attack and death by generating systemic inflammation.
- Comorbidities:
- Chronic kidney disease (CKD): Failing kidneys are not able to effectively remove toxins from the body, which leads to their accumulation and activation of inflammatory processes. A vicious circle is created, the so-called “cardiorenal syndrome”, where damage to one organ drives damage to another.
- Obstructive sleep apnea (OSA): Often an undiagnosed condition, consisting of repeated episodes of stopping or shallow breathing at night. Each such episode leads to hypoxia and rapid stimulation of the sympathetic nervous system, which results in blood pressure spikes, cardiac arrhythmias and increased inflammation. OSA is a significant and independent risk factor for coronary artery disease.
- Gut-heart axis and microbiome: The composition of the gut flora has an impact on heart health. A diet rich in red meat and L-carnitine promotes the growth of bacteria that metabolize these components into trimethylamine (TMA). TMA is converted into trimethylamine N-oxide (TMAO) in the liver. High concentrations of TMAO in the blood promote the development of atherosclerosis and increase platelet reactivity, raising the risk of thrombosis.
- Air pollution: Long-term exposure to smog, especially to small-diameter particulate matter (PM2.5), is a recognized risk factor for heart disease. These tiny particles penetrate from the lungs into the bloodstream, where they cause systemic inflammation, endothelial damage, and increase blood clotting.
- Rare causes of WD: Although atherosclerosis is responsible for most cases, cardiac ischemia can also be caused by spasm of the coronary artery (so-called Prinzmetal angina), embolism (e.g. thrombus from the heart cavities), congenital arterial defects, trauma or inflammatory vascular diseases (eg Kawasaki disease, nodular arteritis is a form of the disease that can lead to myocardial ischemia.
The synergy and convergence of these factors create the “perfect storm” for the development of severe coronary artery disease. An overweight patient, leading a sedentary lifestyle , often develops insulin resistance and type 2 diabetes, which themselves damage the vessels. Obesity is also conducive to the occurrence of obstructive sleep apnea, which puts additional strain on the circulatory system due to nocturnal hypoxia and pressure spikes. If such a patient lives in a polluted city, PM2.5 particulate matter increases systemic inflammation. In this way, seemingly independent factors accumulate and drive each other, leading to a much faster and more severe course of the disease. Understanding this synergy is crucial for effective prevention.
Main risk factors for coronary artery disease and their mechanism of action
| Risk factor | Mechanism of action | Source |
| Smoking | Direct damage to the vascular endothelium, intensification of inflammation, increased blood clotting, acceleration of atherosclerosis. | |
| Hypertension | Mechanical damage to arterial walls, favoring the rupture of atherosclerotic plaques, hypertrophy of the heart muscle. | |
| High LDL cholesterol | The main building block of atherosclerotic plaque; It penetrates the artery wall and initiates the inflammatory process. | |
| Diabetes | Vascular damage by high glucose levels, increased inflammation, favoring dyslipidemia and hypertension. | |
| Obesity / Overweight | It often leads to hypertension, diabetes and lipid disorders; promotes inflammation. | |
| Lack of physical activity | It promotes obesity, hypertension, diabetes; it deteriorates endothelial function and lipid profile. | |
| Chronic stress | Excessive activation of the sympathetic nervous system, increased levels of stress hormones, increased blood pressure and heart rate. | |
| Air pollution (PM2.5) | Penetration into the bloodstream, causing systemic inflammation, endothelial damage, increased blood clotting. |
Symptoms of coronary artery disease – how to recognize the warning signs?
Coronary artery disease can develop secretly for many years without giving any symptoms. However, when the narrowing of the artery becomes large enough to limit the blood supply to the heart, characteristic signals appear. The disease can manifest itself in the form of stable, chronic ailments or as a sudden, life-threatening condition, i.e. acute coronary syndrome.
Typical angina pain: Characteristics, location and what triggers it
The most classic symptom of chronic coronary syndrome is angina pain, also known as angina. Its features are so characteristic that they allow for an initial suspicion of the disease.
- Character and location: Patients describe it as a feeling of crushing, pressure, choking, burning, or a weight located behind the breastbone. This pain is not sharp and stinging, but rather diffuse, which can be a symptom of unstable angina.
- Radiation: The pain often radiates, i.e. spreads, to the neck, jaw, throat, left shoulder and arm, and sometimes to the back (between the shoulder blades) or upper abdomen, which can be mistaken for gastric complaints.
- The factors that cause coronary artery disease can include various health aspects. It typically occurs in situations where the heart has to work harder and needs more oxygen. These are primarily: physical exertion (e.g. fast walking, climbing stairs), severe emotional stress, sudden cooling of the body (going out into the freezing air) or eating a hearty meal.
- Duration and subsidence: Angina pain usually lasts from a few to several minutes (usually 2-5 minutes). A key feature is that it resolves after cessation of exercise (at rest) or after taking sublingually short-acting nitroglycerin. Its severity does not depend on the position of the body or the phase of breathing, which distinguishes it from osteoarticular or pleural pain.
Acute Coronary Syndromes (ACS): When is chest pain a heart attack?
While stable angina is a warning signal, acute coronary syndrome (ACS) is a life-threatening condition. It occurs when the atherosclerotic plaque ruptures and a thrombus forms rapidly on its surface, which partially or completely blocks the coronary artery. The most dangerous form of ACS is a heart attack.
Alarm symptoms that should prompt immediate action include:
- Chest pain: It is much stronger, more severe and extensive than typical angina pain. It can be described as crushing, tearing, or burning.
- Key differentiating feature: Heart attack pain lasts more than 20 minutes and, most importantly, does not go away after rest or after taking nitroglycerin.
- Accompanying symptoms: Pain is often accompanied by other, very disturbing symptoms: severe shortness of breath (feeling of shortness of breath), profuse, cold sweats, feelings of anxiety, panic, fear of death, palpitations, nausea, vomiting, dizziness and even fainting.
If you experience such symptoms , you should not wait or wait for it to “go away on its own”. Call an ambulance immediately by calling 999 or 112. Every minute of delay in treating a heart attack leads to the death of more heart muscle cells and increases the risk of death or permanent disability.
Atypical symptoms of coronary artery disease: angina “masks”, especially in women and diabetics
Coronary artery disease does not always manifest itself in the classic way. Sometimes cardiac ischemia takes on other “masks”, also called “equivalents” of angina. These are symptoms that may not be directly associated with the heart, which makes diagnosis difficult and delayed.
- Exertional dyspnea: This is the most common equivalent of angina pain. The patient feels sudden shortness of breath or difficulty catching their breath during exertion that has not caused them problems so far.
- Other “masks”: These include unusual fatigue and a significant deterioration in exercise tolerance, palpitations, abdominal pain and nausea, and even anxiety and anxiety that occur in connection with physical activity.
There are groups of patients in whom atypical symptoms of the disease are particularly common: the symptoms of ischaemic heart disease may be less obvious.
- Women: Coronary artery disease in women often has a different course than in men. Less often, they experience classic, severe retrosternal pain. Instead, they are more likely to report shortness of breath, unusual fatigue, nausea, indigestion, back, neck, jaw, or arm pain. This is partly due to the fact that in women, the disease is more likely to affect small coronary vessels (so-called microvascular disease) rather than large epicardial arteries.
- Patients with diabetes: Long-term, poorly controlled diabetes leads to damage to nerves, including those responsible for pain sensation (so-called autonomic neuropathy). As a result, patients with diabetes may experience coronary pain very little or not at all. This phenomenon is called “silent ischemia”. A heart attack in a diabetic can be practically painless, and the only symptoms may be sudden weakness, shortness of breath or loss of consciousness.
- Elderly: In seniors, symptoms can also be atypical and are often mistaken for age-related ailments, such as general weakness or impaired consciousness.
Diagnostics – how does the doctor make the diagnosis of coronary artery disease?

Making a correct diagnosis of coronary artery disease requires a comprehensive approach that combines the assessment of symptoms and risk factors with the results of a range of tests, from basic to highly specialized. The diagnostic process has evolved in recent years – from indirect methods, through precise imaging of anatomy, to advanced assessment of the physiology and morphology of lesions in the arteries.
From interview to ECG: First steps in cardiac diagnostics
- Medical history and physical examination: This is the absolute basis and the first step in diagnostics. The doctor collects detailed information about the nature of the complaint (location, radiation, triggers), the presence of risk factors (smoking, hypertension, diabetes, etc.) and the family history of heart disease. Physical examination, including auscultation of the heart and lungs, may provide additional clues.
- Laboratory blood tests: A panel of tests is ordered to assess risk factors and general condition. The key factors are: lipidogram (full cholesterol profile), fasting glucose and glycated hemoglobin (HbA1c) (diabetes diagnosis), creatinine level with eGFR calculation (assessment of kidney function) and C-reactive protein (CRP) (inflammatory marker), which may be associated with the causes of coronary artery disease. In the case of suspected acute coronary syndrome, the key test is the determination of cardiac troponin levels. These are proteins released into the blood from damaged heart muscle cells, and their elevated levels are evidence of a heart attack.
- Resting ECG (electrocardiogram): It’s a simple, cheap and widely available test that records the electrical activity of the heart. It may show signs of a previous infarction, active ischemia or arrhythmias. However, it should be remembered that in many patients with stable coronary artery disease, especially outside of episodes of pain, the ECG recording may be completely normal.
Imaging and functional tests: exercise ECG, echocardiography and CT angio-CT
When basic tests raise the suspicion of CVD, further, more advanced diagnostics are necessary.
- ECG stress test: It involves monitoring ECG and blood pressure during controlled physical exertion, most often on a treadmill or cycloergometer (stationary bike). The goal is to provoke cardiac ischemia that does not occur at rest and record characteristic changes in the ECG. However, this test has its limitations – its result may be unreliable in people who cannot reach the required heart rate due to poor condition or joint diseases.
- Echocardiography (echocardiography): It is an ultrasound examination that allows you to assess the structure and function of the heart in real time. Your doctor can assess the thickness and contractility of individual heart walls, valve function, and left ventricular ejection fraction (heart function index). Segmental contractility disorders may indicate an area of myocardial ischemia.
- Coronary artery angiography (computed tomography): It is a modern, non-invasive imaging test. After intravenous administration of the contrast agent, a series of rapid CT scans synchronized with the heart rate are performed. The obtained images allow for the creation of a three-dimensional reconstruction of the coronary arteries and a very accurate assessment of their anatomy and the presence of stenosis. A high negative predictive value of this test means that a normal result is highly likely to rule out significant coronary artery disease.
Coronary angiography – the “gold standard” and advanced endovascular diagnostics
When non-invasive tests confirm a high probability of the disease or in the case of acute coronary syndromes, coronary angiography is the gold diagnostic standard.
- Coronary angiography (coronary angiography): It is an invasive examination performed in a hemodynamics laboratory. Under local anesthesia, the doctor inserts a thin catheter through the peripheral artery (usually the radial artery on the wrist, less often the femoral artery in the groin) and, under X-ray guidance, guides it all the way to the heart, to the orifices of the coronary arteries. Then, a contrast agent is administered through a catheter, which fills the arteries, and the whole process is recorded on an X-ray film. This examination allows for precise localization of stenosis, assessment of their degree and decision on further treatment – conservative or invasive.
Modern interventional cardiology has tools that allow for an assessment that goes far beyond the angiographic image itself. It is a paradigm shift from the question “is there a stenosis?” to “is this narrowing significant and how is it built?”.
- FFR (Fractional Flow Reserve): Coronary angiography shows anatomy, while FFR evaluates physiology. During the procedure, a special, thin wire with a pressure sensor is inserted through the stenosis. After administration of a maximally vasodilator drug, the pressure before and after the stenosis is measured. The ratio of these pressures (FFR value) objectively determines whether a given stenosis actually restricts blood flow and causes ischaemia. An FFR value of ≤ 0.80 indicates the significance of stenosis and is an indication for intervention. This method avoids unnecessary implantation of stents into lesions that, although visible in angiography, do not impair flow.
- IVUS (Intracoronary Ultrasonography) and OCT (Optical Coherence Tomography): These techniques are a kind of “virtual histology”, allowing you to look inside the artery. IVUS uses a miniature ultrasound probe, and OCT uses infrared light, placed at the end of a catheter inserted into an artery. They allow for an extremely accurate assessment of the vessel wall and the structure of the atherosclerotic plaque (e.g. whether it is soft, rich in lipids, or hard, calcified). This is crucial for planning the procedure (e.g. whether it is necessary to use special techniques to remove calcifications before stent implantation) and for optimizing its result (precise selection of stent size, assessment of its correct adhesion to the vessel wall). OCT, thanks to its ten times higher resolution than IVUS, is particularly valuable in the diagnosis of acute coronary syndromes, allowing to identify subtle plaque ruptures, its erosion or the presence of small thrombi, which is crucial in the diagnosis of myocardial infarctions without significant stenosis in coronary angiography (the so-called MINOCA).
Treatment of Coronary Heart Disease – From Lifestyle Changes to Advanced Procedures
Therapy of coronary artery disease is a comprehensive and long-term process that is based on several pillars. The aim of treatment is not only to alleviate symptoms, but above all to slow down the progression of atherosclerosis, prevent dangerous complications such as heart attack, and improve the quality and length of life of the patient.
Therapy Foundation: Lifestyle Modification and Diet in Coronary Artery Disease
Regardless of the severity of the disease and the treatment methods used, lifestyle change is the absolute basis and condition for the effectiveness of any medical intervention.
- A diet rich in fatty acids may support heart health. Experts unanimously recommend a nutrition model similar to the Mediterranean diet or the DASH diet. They should be rich in vegetables (at least 400 g per day), fruit, wholegrain cereal products, legumes, fish (especially sea, rich in omega-3 acids, eaten at least 2 times a week) and healthy vegetable fats, such as olive oil. At the same time, the consumption of table salt (to less than 5 g, i.e. one flat teaspoon a day), simple sugars, saturated fats (fatty meats, full-fat dairy products) and harmful trans fats present in highly processed foods, sweets and fast food dishes should be drastically reduced.
- Physical activity: According to the guidelines of the European and Polish Society of Cardiology, it is recommended to do at least 150-300 minutes per week of moderate-intensity physical exercise (e.g. brisk walking, cycling, swimming) or 75-150 minutes of high-intensity exercise. A simple and easy-to-remember rule is the “3 x 30 x 130” rule, i.e. training at least 3 times a week, for at least 30 minutes, with an intensity that causes the heart rate to accelerate to about 130 beats per minute.
- Weight reduction: In overweight or obese people, the therapeutic goal is a gradual reduction of body weight, optimally by 5-10% of the baseline value, which brings measurable metabolic and cardiological benefits.
- Smoking cessation and alcohol restriction: Quitting smoking is the single most effective intervention in preventing heart disease. Pharmacological methods are available to support this process, such as nicotine replacement therapy (gums, patches) or drugs (cytisine, varenicline). Alcohol consumption should be significantly reduced.
- Stress management is an important part of the prevention of ischemic heart disease. Chronic stress is a significant risk factor. Relaxation techniques, yoga, and especially the scientifically proven effectiveness of mindfulness-based stress reduction (MBSR) trainings are helpful in reducing it.
Pharmacotherapy: What drugs are used in coronary artery disease and how do they work?
Pharmacological treatment is the second, inseparable element of myocardial infarction therapy. The drugs used can be divided into two main groups: those that improve the prognosis (prolong life) and those that alleviate symptoms (antiangina drugs).
Medications to improve prognosis:
- Antiplatelet drugs: They inhibit the ability of platelets to form blood clots. Acetylsalicylic acid (Aspirin) in a low dose (75-100 mg per day) is the basis of therapy in almost all patients diagnosed with CVD. After the stent implantation procedure, it is necessary to use dual antiplatelet therapy (DAPT) for a certain period of time (from 1 to 12 months, and sometimes longer), i.e. adding a second drug to aspirin, e.g. Clopidogrel, ticagrelor or prasugrel, is used in the prevention of ischaemic heart disease.
- Statins: These are drugs that lower LDL cholesterol levels. Their goal in very high-risk patients (e.g. after a heart attack) is to achieve an LDL value below 1.4 mmol/l (55 mg/dl), which is important in the treatment of ischemic heart disease. Statins are also proven to have anti-inflammatory and stabilizing effects on atherosclerotic plaque, which reduces the risk of its rupture.
- Angiotensin-converting enzyme inhibitors (ACE-I) or sartans (ARBs): They are mandatory in patients with concomitant hypertension, diabetes, heart failure or after a heart attack. These drugs lower blood pressure, relieve the heart and protect it from adverse remodeling.
Antiangina (symptomatic):
- Beta-blockers are often used to treat the symptoms of coronary heart disease. They slow down the heart rate and lower blood pressure, thus reducing the demand of the heart muscle for oxygen, which is crucial in the treatment of ischemic heart disease. They are the first choice drugs for the treatment of angina and improve exercise tolerance.
- Calcium channel blockers: They dilate the arteries (both coronary and peripheral), lowering pressure and improving blood supply to the heart. They can be used alone or in combination with beta-blockers.
- Nitrates: Short-acting nitroglycerin (in the form of an aerosol or sublingual tablets) is used to temporarily interrupt an attack of angina pain – it works within several dozen seconds. Long-acting nitrates are used in regular therapy to prevent pain.
- Second-line drugs: When the above medications are insufficient or poorly tolerated, your doctor may include other preparations such as trimetazidine, ivabradine, ranolazine or nicorandil to improve blood circulation to the heart muscle.
Main groups of drugs in coronary artery disease and their role
| A group of drugs | Examples | Key Action | Role in therapy |
| Antiplatelet drugs | Acetylsalicylic acid, clopidogrel, ticagrelor are crucial in the treatment and prevention of ischemic heart disease. | Inhibition of platelet aggregation | Improved prognosis: Prevention of thrombosis in the arteries and stents, prevention of myocardial infarction. |
| Statins | Atorvastatin, rosuvastatin | Lowering LDL cholesterol, stabilizing atherosclerotic plaque, anti-inflammatory effect | Improved prognosis: Slowing down the progression of atherosclerosis, reducing the risk of heart attack and stroke. |
| ACE Inhibitors / Sartans | Ramipril, perindopril / Valsartan, telmisartan | Lowering blood pressure, relieving the heart, protection against left ventricular remodeling | Improved prognosis: Especially in patients with hypertension, diabetes, heart failure. |
| Beta-blockers | Metoprolol, bisoprolol, carvedilol | Slowing down the heart rate, lowering blood pressure, and reducing the heart’s demand for oxygen are important in the context of myocardial ischemia. | Symptomatic treatment + Improvement of prognosis (especially after myocardial infarction and heart failure). |
| Calcium channel blockers | Amlodipine, diltiazem, verapamil | Arterial dilation, lowering blood pressure | Symptomatic: Reduction of angina pain. |
| Nitrates | Nitroglycerin, isosorbide mononitrate | Vasodilation (mainly venous), reduced load on the heart | Symptomatic: Emergency pain relief (short-acting), prophylaxis (long-acting). |
Invasive treatment: Angioplasty (ballooning, stents) and bypasses
In a situation where pharmacological treatment is insufficient to control the symptoms or when stenosis in the coronary arteries is critical and poses a high risk of infarction, invasive treatment, i.e. myocardial revascularization, is necessary.
- Percutaneous Coronary Intervention (PCI): This is a commonly used, minimally invasive method, commonly known as “ballooning” or “stenting”. The procedure is performed in the hemodynamics laboratory, most often immediately after the diagnosis of ischemic heart disease. Through the same catheter, a guidewire with a balloon is inserted at the site of the stenosis. Expansion of the balloon under high pressure causes the atherosclerotic plaque to “crush” and widen the lumen of the artery. Then, in the vast majority of cases, a stent is implanted in the same place – it is a small, reticulate, metal tube (resembling a spring), which acts as a “scaffold” for the vessel wall and prevents it from narrowing again (restenosis).
- Coronary Artery Bypass Grafting (CABG): It is a cardiac surgery, popularly known as “bypasses”. It is used in the case of more advanced, multivessel coronary artery disease, in the case of stenosis of the left coronary artery trunk or when the anatomy of the lesions is unfavorable for PCI, which is important in the treatment of ischemic heart disease. The procedure involves the creation of a “bypass” bypassing the narrowed section of the artery. As a bypass, the surgeon uses blood vessels taken from the patient himself – most often it is the internal thoracic artery (which has the best long-term patency) or a fragment of the saphenous vein taken from the leg. One end of the bypass is sewn into the aorta (the main artery of the body) and the other end into the coronary artery behind the site of stenosis. In this way, the blood bypasses the obstacle and freely reaches the heart muscle. This method is particularly preferred in patients with diabetes and multivessel disease, as it gives better long-term results than PCI in this group.
Living with Coronary Heart Disease – Secondary Prevention and Rehabilitation
The diagnosis of coronary artery disease, a history of myocardial infarction or an invasive procedure is not the end of treatment, but on the contrary – the beginning of a new stage in which the patient himself plays a key role. Secondary prevention, i.e. actions taken after a cardiac event, aims to prevent recurrence of the disease and improve the quality of life. Its foundation is strict adherence to recommendations, which in medicine is referred to as adherence.
Life after infarction and angioplasty: Key recommendations and cardiac rehabilitation
- Key recommendations after the PCI procedure: After stent implantation, it is absolutely critical to take medication regularly, especially dual antiplatelet therapy (aspirin + second drug). Its sudden discontinuation threatens with catastrophic closure of the stent by a clot (the so-called stent thrombosis is a serious complication that can lead to myocardial infarction. In the first week after the procedure, you should avoid lifting weights and intense physical exertion, and observe the injection site (on the wrist or groin) for bleeding, swelling or pain.
- Comprehensive cardiac rehabilitation: It is a structured, multifaceted therapeutic program that is an integral part of treatment after a heart attack, angioplasty or bypass surgery. It includes individually planned and supervised physical training, education about the disease, modification of risk factors, dietary advice and psychological support.
- Stages of rehabilitation: This process is divided into three main stages. Stage I begins in the hospital, a few days after the acute incident. Stage II, crucial for recovery, usually lasts from 4 to 12 weeks and can be carried out in inpatient conditions (in a cardiac rehabilitation ward), outpatient (daily commuting to exercises) or, in selected cases, at home under the supervision of specialists. Stage III is basically secondary prevention continued throughout life, consisting in consolidating healthy habits.
- Benefits of rehabilitation: Participation in a cardiac rehabilitation program significantly reduces the risk of further heart attacks, hospitalization and death. It improves physical performance, allows you to safely return to professional and social activity and increases the quality of life.
KOS-Zawał Program: What is comprehensive care after a heart attack in Poland?
In order to address the problem of dispersed and often insufficient care after a heart attack, in 2017 a program of Comprehensive Specialist Care after a Heart Attack (KOS-Zafar) financed by the National Health Fund was introduced in Poland.
- Program assumptions: The idea of KOS-Zafart is to provide continuous and coordinated care to the patient for 12 months from the moment of the infarction. The program is to ensure that the patient “does not disappear from the system” after leaving the hospital.
- Program elements: A patient qualified for the program in the hospital where he or she was treated is guaranteed:
- Full interventional treatment of the acute phase of infarction.
- Comprehensive cardiac rehabilitation (stationary or day).
- Implantation of electrotherapy devices (pacemaker, cardioverter-defibrillator), if indicated.
- One-year, unlimited care in a cardiology clinic, with at least 4 follow-up visits, including a balance of care at the end of the program.
- Effectiveness: The data of the National Health Fund clearly show that the program is a success. Patients with KOS-Infarction have a much better prognosis and a lower risk of death, and the percentage of people using rehabilitation, which is crucial for health, is many times higher in this group. By the end of 2022, more than 68 thousand patients had benefited from the program.
Psychological aspects: How to deal with anxiety and depression after diagnosis?
A heart attack is a traumatic experience that leaves a mark not only on the body, but also on the psyche. Anxiety, a sense of helplessness, depression and loss of interest are common reactions.
- Depression and anxiety as risk factors: It is estimated that clinically significant depressive symptoms occur in up to 40-65% of patients after a heart attack. Importantly, depression is not just a “malaise” – it is an independent factor that worsens the prognosis. It increases the risk of subsequent cardiovascular events by about 30%. This is for two reasons: first, patients with depression are less likely to adhere to medical recommendations; Secondly, depression has a direct, negative biological impact – it increases inflammation in the body and increases the activity of platelets, which promotes thrombosis.
- Treatment and support: Mental problems after a heart attack can and should be treated. Both pharmacotherapy (SSRIs are considered safe in cardiac patients) and psychotherapy (e.g. in people with ischaemic heart disease) are effective. cognitive-behavioral therapy). Family support and the opportunity to talk to other people who have gone through similar experiences are extremely important.
Unfortunately, adherence to therapeutic recommendations is one of the greatest, although often underestimated, challenges in the treatment of chronic diseases. State-of-the-art therapies are ineffective if the patient does not use them. The data is alarming – in Poland, up to 58% of patients with hypertension and every second patient after a heart attack do not fully implement the treatment plan. What’s more, a year after a heart attack, the percentage of patients taking drugs from all three key therapeutic groups drops by as much as 70%. The causes of this phenomenon are complex: from a lack of understanding of the essence of the disease, through fear of adverse effects, to psychological factors, such as depression. This low health awareness and lack of a sense of co-responsibility for the treatment process lead to tragic consequences. That is why education, building a partnership relationship with the doctor and actively involving the patient in therapy are so crucial.
Where to look for support? Patient organizations and hotlines in Poland
Patients and their families are not left alone. There are several organizations in Poland that offer reliable knowledge, psychological support and help in navigating the health care system:
- The Polish Association of People with Heart Failure (nspacjenci.pl) deals with, among m.in, disease prevention and support for patients with symptoms of ischaemic heart disease. A formal support group for patients with heart failure and their relatives, operating under the auspices of the PCS Heart Failure Section.
- Association “ICDefibrillators” (icd.org.pl): An organization associating and supporting patients with implanted cardiac devices (pacemakers, cardioverter-defibrillators).
- National Association of Patients with Heart and Vascular Diseases “EcoSerce” (ecoserce.pl): An association fighting for the rights of cardiac patients and raising public awareness.
- Cardioline (kardiolinia.pl): The Centre for Education and Support for Patients with Heart Failure, offering free educational advice provided by telephone by specialist nurses and educators.
Special Issues and the Future of Cardiology
Cardiology is one of the most dynamically developing fields of medicine, especially in the context of ischemic heart disease in Poland. Progress is not only about improving known therapies, but also about discovering new disease entities and introducing revolutionary technologies that change the face of diagnostics and treatment.
Spontaneous coronary artery dissection (SCAD): Heart attack in young women
For years considered rare, today spontaneous coronary artery dissection (SCAD) is recognized as a significant, non-atherosclerotic cause of myocardial infarction, especially in young (<50 years of age) and previously healthy women, often without classic risk factors.
- The essence of the disease: SCAD consists of a spontaneous rupture of the coronary artery wall, unrelated to injury or medical procedure. This leads to the formation of a hematoma inside the vessel wall, which presses its lumen and restricts blood flow, causing ischemia and infarction.
- Causes and triggers: SCAD often coexists with fibromuscular dysplasia (FMD) – another non-inflammatory, non-atherosclerotic arterial disease. Factors that can trigger dissection include, m.in, severe emotional or physical stress, as well as hormonal changes associated with pregnancy and the postpartum period.
- Diagnosis and treatment: The diagnosis is made on the basis of a characteristic picture in coronary angiography, often supported by the diagnosis of ischemic heart disease, intracoronary imaging (OCT, IVUS). The management of SCAD differs from the treatment of atherosclerotic infarction. Since dissected arteries have a high capacity for self-healing, conservative (pharmacological) treatment is preferred in stable cases. Invasive treatment (PCI, CABG) is reserved for unstable patients, with persistent ischemia or life-threatening cardiac arrhythmias, which may be the cause of ischemic heart disease.
New horizons in treatment: From PCSK9 inhibitors to gene therapies
- A revolution in the treatment of hypercholesterolemia: For patients in whom statins in maximum doses are insufficient to achieve the therapeutic goal or are poorly tolerated, biological drugs – PCSK9 inhibitors (evolocumab, alirocumab) turned out to be a breakthrough. These are monoclonal antibodies, administered in the form of subcutaneous injections (once every 2 or 4 weeks), which block the PCSK9 protein responsible for the breakdown of receptors for “bad” LDL cholesterol. The result is a drastic reduction in LDL concentration, reaching 50-70%. An even newer option is Inclisiran is a new drug that can be used to treat people with coronary heart disease., a drug based on small interfering RNA (siRNA) technology that “switches off” the production of the PCSK9 protein in liver cells. Its great advantage is the dosage schedule – after the initial dose and the next dose after 3 months, the next injections are administered only twice a year.
- Regenerative therapies: The holy grail of cardiology is the repair of a heart damaged by a heart attack. Intensive research is currently underway on cell therapies (using different types of stem cells) and gene therapies. The latter, using, for example, mRNA technology (known from COVID-19 vaccines), are aimed at delivering genetic factors to heart cells that will stimulate them to divide and regenerate. Animal studies show promising results and give hope that in the future it will be possible to fully rebuild the heart muscle.
Artificial intelligence (AI) and personalized medicine in heart diagnostics
- AI in cardiac diagnostics: Artificial intelligence is already revolutionizing cardiology. AI algorithms are able to analyze ECG, echocardiography, computed tomography or magnetic resonance imaging images faster and often with greater precision than the human eye, detecting subtle patterns invisible to the doctor. In Poland, the PZU Zdrowie network has already implemented the Cardiomatics system, based on AI, for automatic analysis of ECG tests using the Holter method. In the future, AI will be able to predict the risk of a heart attack based on a huge amount of data, including genetic factors, lifestyle and even air pollution levels.
- Pharmacogenomics – tailor-made treatment: It is a field that deals with the selection of drugs based on the genetic profile of the patient. A great example is the use of clopidogrel. It is a prodrug, which means that it must be activated in the body by liver enzymes, mainly in the context of treating ischemic heart disease. CYP2C19. Part of the population (about 30% in Europe) has genetic variants of this enzyme that cause its weaker effect (the so-called loss-of-function variants). In such patients, clopidogrel is not effectively activated, leading to weaker platelet inhibition and significantly increasing the risk of stent thrombosis after angioplasty. A simple genetic test can identify these patients and indicate the need for another, stronger antiplatelet drug (e.g. ticagrelor) from the beginning, which does not require activation by the CYP2C19. This is a real example of personalized medicine in practice.
Your Heart in Your Hands – The Key to a Long and Healthy Life
Coronary artery disease is a chronic and progressive disease that poses one of the greatest threats to the health and life of Poles. However, the diagnosis is not a sentence. Modern medicine offers a wide range of effective diagnostic and therapeutic methods, from lifestyle changes, through advanced pharmacotherapy, to minimally invasive procedures and cardiac surgery.
The key to success in the fight against this disease is to understand that it is based on three pillars. The first is conscious prevention – a healthy diet, regular physical activity, maintaining a healthy body weight, not smoking cigarettes and coping with stress are the most powerful weapons we have at our disposal to slow down or even stop the progression of atherosclerosis. The second pillar is early diagnosis – you should not ignore alarming symptoms, such as chest pain or shortness of breath due to exertion, especially if you belong to the risk group. The third, and perhaps the most important pillar after diagnosis, is close cooperation with the doctor and systematic adherence to recommendations. Regular medication, participation in rehabilitation and periodic check-ups are an investment in your own health, which brings measurable benefits in the form of a longer life in better condition.
Progress in cardiology is extremely dynamic. New drugs, innovative surgical techniques, artificial intelligence and personalized medicine are opening up prospects for patients that seemed like science fiction a decade ago. However, no technology, even the most modern one, can replace the fundamental role played by the patient himself. Your heart is in your hands, and knowledge and responsibility are the most effective tools in the fight for a long and healthy life.